🧠💥 Intraparenchymal Hemorrhage (IPH) – High-Yield Summary
Definition:
Spontaneous bleeding into brain parenchyma, causing direct tissue injury 🧩, mass effect, and secondary damage via edema 💧, inflammation 🧬, oxidative stress ⚡. Accounts for ~10–15% of strokes, highest mortality among stroke subtypes.
🔹 Pathophysiology 🧬
- Primary Injury:
- Rupture of small deep penetrating arteries 🩸 → hematoma formation
- Direct tissue destruction 🧠 + mass effect → increased ICP 📊
- Secondary Injury Cascade:
- Perihematomal edema 💧
- Inflammatory response 🧪
- Cytotoxic enzyme release 🧬
- Oxidative stress ⚡ → further neurological deterioration
🔹 Etiology & Risk Factors 🩺
1️⃣ Vascular Causes:
- Hypertension 🩸 – 50–60% (lipohyalinosis, fibrinoid necrosis)
- Cerebral Amyloid Angiopathy (CAA) 🧪 – especially elderly, lobar bleeds
2️⃣ Structural & Other Causes:
- Vascular malformations: AVMs, cavernomas 🌐
- Tumors 🧬
- Coagulopathies (inherited or iatrogenic ⚗️)
- Cerebral venous thrombosis
- Sympathomimetic drugs 💊
3️⃣ Modifiable Risk Factors:
- Chronic hypertension 🩸
- Excessive alcohol 🍷
- Anticoagulant therapy 💊
🔹 Clinical Presentation & Diagnosis ⚡
Symptoms:
- Sudden severe headache 🤕
- Nausea / vomiting 🤢
- Focal neurological deficits (location-dependent 🧠)
- Rapidly declining consciousness 🛌
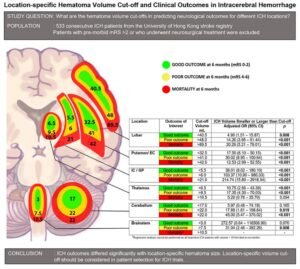
Examples by Location:
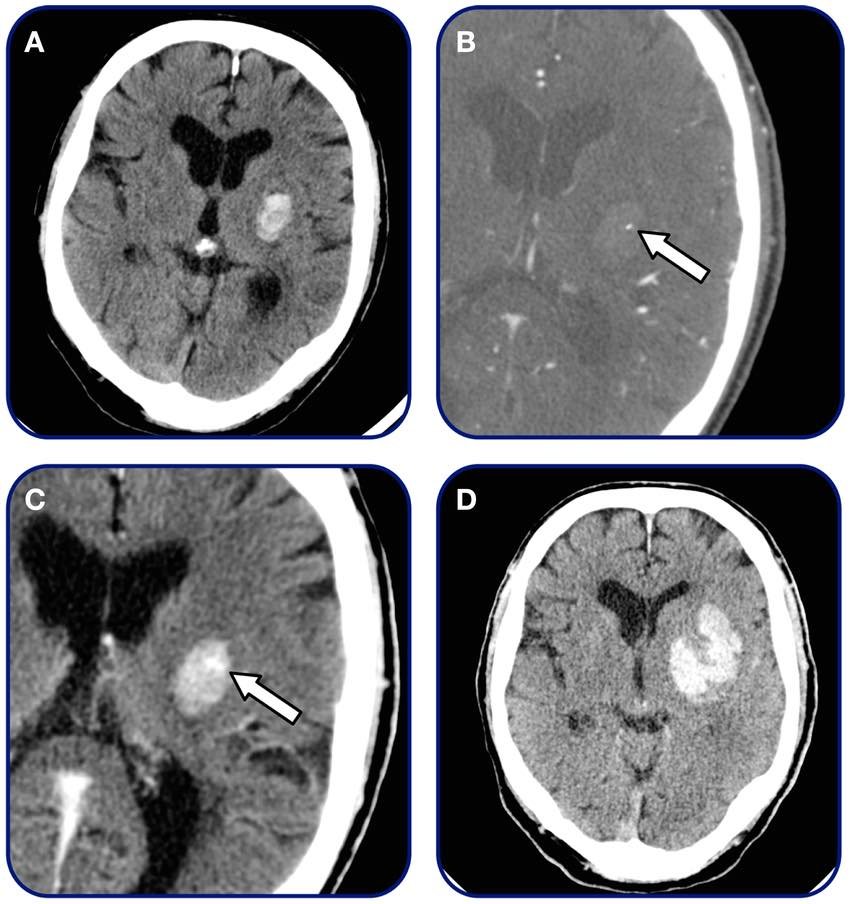
- Putamen: contralateral hemiparesis ✋
- Thalamus: sensory loss, vertical gaze palsy 👀
- Cerebellum: ataxia, nystagmus, dizziness 🤸♂️
- Brainstem (pontine): coma, decerebrate posturing 🛌
Investigations 🖥️:
- Non-contrast CT: first-line, hyperdense blood
- MRI (GRE / SWI): detect underlying lesions
- CT Angiography (CTA): vascular anomalies, “spot sign” predicts expansion
- CSF / Labs: if infection or coagulopathy suspected
🔹 Management 🏥
1️⃣ Medical Management:
- ICU monitoring 🏥
- Aggressive BP control 🩸 (target <140 mmHg)
- Coagulopathy reversal ⚗️: vitamin K, PCC, FFP, DOAC reversal
- ICP management 🧠: head elevation, mannitol / hypertonic saline, sedation
2️⃣ Surgical Management ⚒️:
- Cerebellar hemorrhage >3 cm with deterioration → urgent evacuation
- Supratentorial hemorrhage: evidence limited; STICH trials show selective benefit
- Minimally invasive techniques 🧬: stereotactic aspiration + thrombolysis under study
🔹 Prognosis & Outcomes 📊
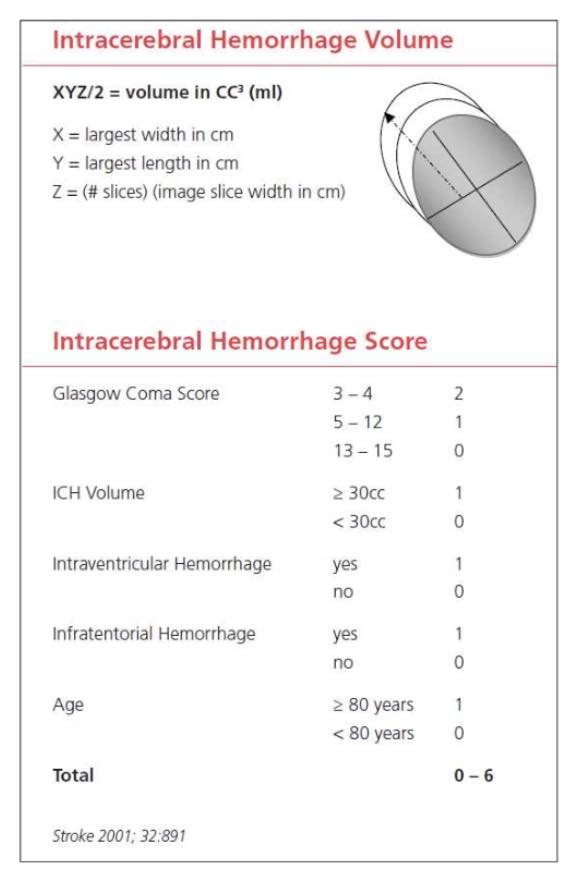
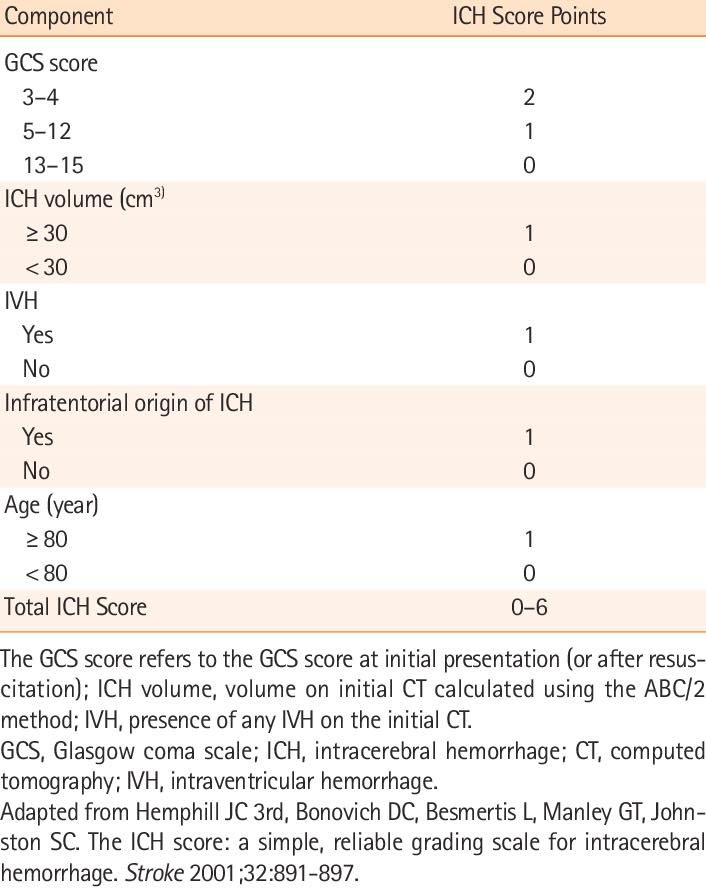
- 30-day mortality: ~40% (half in first 48 hours)
- Poor prognostic factors:
- Advanced age 👵👴
- Low GCS at presentation
- Large hematoma volume 🧠
- Intraventricular extension
- Infratentorial location
- Ongoing anticoagulation 💊
- Survivors: significant disability
- Persistent motor, sensory, cognitive, speech deficits
- Long-term rehab often required 🏋️♂️
- Measured with modified Rankin Scale 📏
💡 Key Pearls
Surgery mainly for cerebellar or superficial lobar hemorrhages ⚒️
Hypertension = most common modifiable cause 🩸
CT scan 🖥️ = first-line rapid diagnosis
Hematoma volume & location predict prognosis 📊
Early detection & BP control ↓ hematoma expansion