🧠🩸 Intraventricular Hemorrhage (IVH) in the NeuroICU – Comprehensive Review
📌 I. Introduction
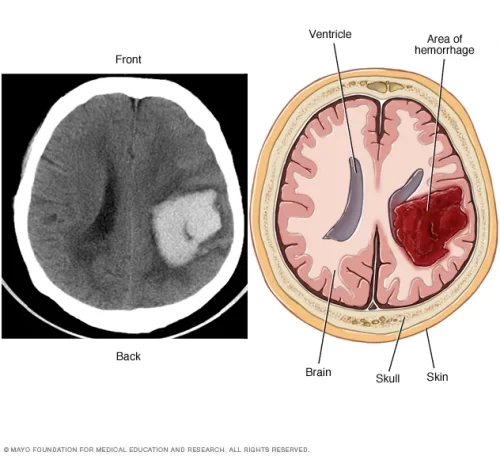
- IVH = bleeding into the cerebral ventricular system
- Historically fatal; modern NeuroICU care 💉 improves outcomes
- Mortality: 30–50% in severe cases
- Mechanisms:
- ➡️ Extension from parenchymal hemorrhage (45–50%)
- 🧫 Primary intraventricular bleeding (20–30%)
- 🌊 Subarachnoid hemorrhage with ventricular reflux (20–25%)
📊 II. Classification Systems
🟢 Graeb Scale (0–12)
- 0: No blood
- 1–4: Trace to mild (<50% of ventricle)
- 5–8: Moderate (≥50%)
- 9–12: Severe (ventricle expanded)
🔵 Modified Graeb Scale (mGS, 0–16)
- More precise for clot volume
- Lateral ventricles: 1 pt per 25% filling (0–4 each)
- Third/fourth ventricles: 1 pt per 25% filling
🟡 LeRoux Scale
- Clot size + hydrocephalus per ventricle
- Separate hemorrhage & hydrocephalus scores
🔴 IVH Score (0–3)
- 1 pt each for: blood in 3rd, 4th, lateral ventricles
- Higher = worse prognosis
🔬 III. Pathophysiology
⚡ Primary Injury Mechanisms
- 🧠 Mass Effect & ↑ICP: Direct clot expansion
- 🔥 Chemical Ependymitis: Blood degradation products → ependymal inflammation
- 🚰 Obstructive Hydrocephalus: Clot blocks
- Foramina of Monro → unilateral hydrocephalus
- Cerebral Aqueduct → tricompartmental hydrocephalus
- 4th ventricle outlets → transependymal CSF flow
- 💧 Periventricular Edema: Ischemic injury
🧪 Secondary Injury Cascade
- 🧬 Inflammation: Microglia, IL-1β, TNF-α
- ⚡ Oxidative stress: Hemoglobin → iron-mediated free radicals
- 🧱 BBB disruption: VEGF → vasogenic edema
- 🩸 Cerebral hypoperfusion: Autoregulation failure
🔋 Metabolic Changes
- 🌡️ Global CBF ↓ 50% in severe IVH
- 🌀 Periventricular “penumbra”
- 🍬 CSF: lactate ↑, pH ↓, glucose ↓
🧩 IV. Etiologies & Clinical Presentations
🏥 Primary IVH
- 🩺 Hypertensive hemorrhage (40–50%) – thalamus, basal ganglia
- 🧬 AVMs (10–15%)
- 🏗️ Cavernomas (5%) – subependymal
- 🎯 Tumors (3–5%) – choroid plexus, metastases
- 💉 Coagulopathies (10%) – anticoagulants, thrombocytopenia
- 🧓 Cerebral amyloid angiopathy (elderly)
- 🌊 Venous infarction
⚠️ Secondary IVH
- 🩸 SAH with ventricular extension (PCOM, ACOM, basilar tip)
- 🚑 Traumatic IVH
- 🔄 Hemorrhagic transformation of ischemic stroke
- 🧬 Moyamoya disease
🌡️ Clinical Spectrum
- 💥 Catastrophic: sudden headache → coma (Graeb 8–12)
- ⏳ Subacute: progressive headache, nausea, lethargy
- 🖐️ Focal: deficits depending on primary hemorrhage
- 🚰 Hydrocephalic: headache + vomiting + lethargy
🧪 V. Diagnostic Evaluation
🖥️ Neuroimaging
- 🩻 Non-contrast CT: gold standard
- Quantify volume (mGS ≥5 → poor prognosis)
- Assess parenchymal component, mass effect, hydrocephalus
- Signs: “Cast” (ventricles filled), “Swirl” (active bleeding)
- 🌉 CT Angiography: detect AVM/aneurysm, “spot sign” predicts expansion
- 🧲 MRI (GRE/SWI/DWI/FLAIR): microbleeds, cavernomas, ischemia, transependymal flow
- 🔍 DSA: for negative CTA with high suspicion, repeat in 6–8 weeks if needed
💧 Cerebrospinal Fluid Analysis
- 💉 Lumbar puncture: therapeutic + diagnostic in communicating hydrocephalus
- CSF: xanthochromia, ↑ protein, pleocytosis
- Drainage: 20–30 mL/hr; monitor opening pressure
🧰 NeuroICU Monitoring
- 🚰 EVD: ICP monitoring + CSF drainage
- Level at tragus, drain 10–15 cm H₂O
- Complications: infection 5–20%, hemorrhage 2–5%, malfunction
- 🌡️ Multimodality Monitoring
- PbtO₂ >20 mmHg
- Cerebral microdialysis: LPR <25, glucose >0.8 mmol/L
- Continuous EEG: detect non-convulsive seizures (10–20%)